Abstract
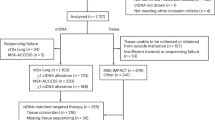
The natural history of small-cell lung cancer (SCLC) includes rapid evolution from chemosensitivity to chemoresistance, although mechanisms underlying this evolution remain obscure due to the scarcity of post-relapse tissue samples. We generated circulating tumor cell (CTC)-derived xenografts from patients with SCLC to study intratumoral heterogeneity (ITH) via single-cell RNA sequencing of chemosensitive and chemoresistant CTC-derived xenografts and patient CTCs. We found globally increased ITH, including heterogeneous expression of therapeutic targets and potential resistance pathways, such as epithelial-to-mesenchymal transition, between cellular subpopulations following treatment resistance. Similarly, serial profiling of patient CTCs directly from blood confirmed increased ITH post-relapse. These findings suggest that treatment resistance in SCLC is characterized by coexisting subpopulations of cells with heterogeneous gene expression leading to multiple, concurrent resistance mechanisms. These findings emphasize the need for clinical efforts to focus on rational combination therapies for treatment-naïve SCLC tumors to maximize initial responses and counteract the emergence of ITH and diverse resistance mechanisms.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The single-cell and bulk RNA-Seq data have been deposited in the NCBI Gene Expression Omnibus database with accession number GSE138474. Source data for Figs. 1–6 and Extended Data Figs. 1–6 are provided with the paper. All other data supporting the findings of this study are available from the corresponding author upon reasonable request.
Code availability
The bioinformatics analyses were performed using open-source software, including BWA-MEM version 0.7.9a49, VARSCAN2 version 2.3.9 (ref. 50), TOPHAT2 version 2.0.13 (ref. 51), HTSEQ version 0.9.1 (ref. 52), EdgeR version 3.7 (ref. 53), GSEA version 3.0 (ref. 42), ANNOVAR version 2018Apr16 (ref. 54), Seurat version 2.3 (ref. 55) and Cell Ranger version 2.0, as well as in-house R script that is available upon request.
References
Horn, L. et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N. Engl. J. Med. 379, 2220–2229 (2018).
H.R.733: Leech Lake Band of Ojibwe Reservation Restoration Act (Senate and House of Representatives of the United States of America in Congress, 2012). https://www.congress.gov/bill/112th-congress/house-bill/733
Hodgkinson, C. L. et al. Tumorigenicity and genetic profiling of circulating tumor cells in small-cell lung cancer. Nat. Med. 20, 897–903 (2014).
Drapkin, B. J. et al. Genomic and functional fidelity of small cell lung cancer patient-derived xenografts. Cancer Discov. 8, 600–615 (2018).
Chalishazar, M. D. et al. MYC-driven small-cell lung cancer is metabolically distinct and vulnerable to arginine depletion. Clin. Cancer Res. 25, 5107–5121 (2019).
Aggarwal, C. et al. Circulating tumor cells as a predictive biomarker in patients with small cell lung cancer undergoing chemotherapy. Lung Cancer 112, 118–125 (2017).
Farago, A. F. et al. Combination olaparib and temozolomide in relapsed small-cell lung cancer. Cancer Discov. 9, 1372–1387 (2019).
Zhang, J. et al. Intratumor heterogeneity in localized lung adenocarcinomas delineated by multiregion sequencing. Science 346, 256–259 (2014).
Mollaoglu, G. et al. MYC drives progression of small cell lung cancer to a variant neuroendocrine subtype with vulnerability to aurora kinase inhibition. Cancer Cell 31, 270–285 (2017).
Huang, Y. H. et al. POU2F3 is a master regulator of a tuft cell-like variant of small cell lung cancer. Genes Dev. 32, 915–928 (2018).
Cardnell, R. J. et al. Protein expression of TTF1 and cMYC define distinct molecular subgroups of small cell lung cancer with unique vulnerabilities to aurora kinase inhibition, DLL3 targeting, and other targeted therapies. Oncotarget 8, 73419–73432 (2017).
Lim, J. S. et al. Intratumoural heterogeneity generated by Notch signalling promotes small-cell lung cancer. Nature 545, 360–364 (2017).
Shue, Y. T., Lim, J. S. & Sage, J. Tumor heterogeneity in small cell lung cancer defined and investigated in pre-clinical mouse models. Transl. Lung Cancer Res. 7, 21–31 (2018).
Tirosh, I. et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-Seq. Science 352, 189–196 (2016).
Skoulidis, F. et al. Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer Discov. 5, 860–877 (2015).
Rudin, C. M. et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat. Rev. Cancer 19, 289–297 (2019).
Misch, D. et al. Value of thyroid transcription factor (TTF)-1 for diagnosis and prognosis of patients with locally advanced or metastatic small cell lung cancer. Diagn. Pathol. 10, 21 (2015).
Zhang, W. et al. Small cell lung cancer tumors and preclinical models display heterogeneity of neuroendocrine phenotypes. Transl. Lung Cancer Res. 7, 32–49 (2018).
George, J. et al. Comprehensive genomic profiles of small cell lung cancer. Nature 524, 47–53 (2015).
Jahchan, N. S. et al. Identification and targeting of long-term tumor-propagating cells in small cell lung cancer. Cell Rep. 16, 644–656 (2016).
Singhi, A. D. et al. MYC gene amplification is often acquired in lethal distant breast cancer metastases of unamplified primary tumors. Mod. Pathol. 25, 378–387 (2012).
Lee, H. Y. et al. c-MYC drives breast cancer metastasis to the brain, but promotes synthetic lethality with TRAIL. Mol. Cancer Res. 17, 544–554 (2019).
Stewart, C. A. et al. Dynamic variations in epithelial-to-mesenchymal transition (EMT), ATM, and SLFN11 govern response to PARP inhibitors and cisplatin in small cell lung cancer. Oncotarget 8, 28575–28587 (2017).
Gardner, E. E. et al. Chemosensitive relapse in small cell lung cancer proceeds through an EZH2–SLFN11 axis. Cancer Cell 31, 286–299 (2017).
Wagner, A. H. et al. Recurrent WNT pathway alterations are frequent in relapsed small cell lung cancer. Nat. Commun. 9, 3787 (2018).
Byers, L. A. et al. Proteomic profiling identifies dysregulated pathways in small cell lung cancer and novel therapeutic targets including PARP1. Cancer Discov. 2, 798–811 (2012).
Dammert, M. A. et al. MYC paralog-dependent apoptotic priming orchestrates a spectrum of vulnerabilities in small cell lung cancer. Nat. Commun. 10, 3485 (2019).
Semenova, E. A. et al. Transcription factor NFIB is a driver of small cell lung cancer progression in mice and marks metastatic disease in patients. Cell Rep. 16, 631–643 (2016).
Bottger, F. et al. Tumor heterogeneity underlies differential cisplatin sensitivity in mouse models of small-cell lung cancer. Cell Rep. 27, 3345–3358.e4 (2019).
Wu, N. et al. NFIB overexpression cooperates with Rb/p53 deletion to promote small cell lung cancer. Oncotarget 7, 57514–57524 (2016).
Klameth, L. et al. Small cell lung cancer: model of circulating tumor cell tumorospheres in chemoresistance. Sci. Rep. 7, 5337 (2017).
Hamilton, G., Hochmair, M., Rath, B., Klameth, L. & Zeillinger, R. Small cell lung cancer: circulating tumor cells of extended stage patients express a mesenchymal–epithelial transition phenotype. Cell Adh. Migr. 10, 360–367 (2016).
Yu, N., Zhou, J., Cui, F. & Tang, X. Circulating tumor cells in lung cancer: detection methods and clinical applications. Lung 193, 157–171 (2015).
Tanaka, F. et al. Circulating tumor cell as a diagnostic marker in primary lung cancer. Clin. Cancer Res. 15, 6980–6986 (2009).
Rudin, C. M. et al. Rovalpituzumab tesirine, a DLL3-targeted antibody–drug conjugate, in recurrent small-cell lung cancer: a first-in-human, first-in-class, open-label, phase 1 study. Lancet Oncol. 18, 42–51 (2017).
Giffin, M. et al. Targeting DLL3 with AMG 757, a BiTE® antibody construct, and AMG 119, a CAR-T, for the treatment of SCLC. J. Thorac. Oncol. 13, abstr. P3.12-03 (2018).
Carbone, D. P. et al. Efficacy and safety of rovalpituzumab tesirine in patients with DLL3-expressing, ≥ 3rd line small cell lung cancer: results from the phase 2 TRINITY study. J. Clin. Oncol. 36(Suppl.), 8507 (2018).
Paz-Ares, L. et al. Overall survival with durvalumab plus etoposide–platinum in first-line extensive-stage SCLC: results from the CASPIAN study. J. Thorac. Oncol. 14, S7–S8 (2019).
Nugent, J. L. et al. CNS metastases in small cell bronchogenic carcinoma: increasing frequency and changing pattern with lengthening survival. Cancer 44, 1885–1893 (1979).
Butler, A., Hoffman, P., Smibert, P., Papalexi, E. & Satija, R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat. Biotechnol. 36, 411–420 (2018).
Jamieson, A. R. et al. Exploring nonlinear feature space dimension reduction and data representation in breast CADx with laplacian eigenmaps and t-SNE. Med. Phys. 37, 339–351 (2010).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
McCarthy, D. J., Chen, Y. & Smyth, G. K. Differential expression analysis of multifactor RNA-Seq experiments with respect to biological variation. Nucleic Acids Res. 40, 4288–4297 (2012).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Tong, P., Chen, Y., Su, X. & Coombes, K. R. SIBER: systematic identification of bimodally expressed genes using RNAseq data. Bioinformatics 29, 605–613 (2013).
Wang, J., Wen, S., Symmans, W. F., Pusztai, L. & Coombes, K. R. The bimodality index: a criterion for discovering and ranking bimodal signatures from cancer gene expression profiling data. Cancer Inform. 7, 199–216 (2009).
Byers, L. A. et al. An epithelial–mesenchymal transition gene signature predicts resistance to EGFR and PI3K inhibitors and identifies Axl as a therapeutic target for overcoming EGFR inhibitor resistance. Clin. Cancer Res. 19, 279–290 (2013).
R Core Development Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2015).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows–Wheeler transform. Bioinformatics 26, 589–595 (2010).
Koboldt, D. C. et al. VarScan: variant detection in massively parallel sequencing of individual and pooled samples. Bioinformatics 25, 2283–2285 (2009).
Kim, D. et al. TopHat2: accurate alignment of transcriptomes in the presence of insertions, deletions and gene fusions. Genome Biol. 14, R36 (2013).
Anders, S., Pyl, P. T. & Huber, W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinformatics 31, 166–169 (2015).
Dai, Z. et al. edgeR: a versatile tool for the analysis of shRNA-Seq and CRISPR–Cas9 genetic screens. F1000Res 3, 95 (2014).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177, 1888–1902.e21 (2019).
Acknowledgements
We thank the patients who participated in this study, as well as their families. We also thank M. Vasquez for obtaining consent from the patients, E. Roarty for scientific input and editing, and K. Ramkumar for general laboratory assistance. This work was supported by NIH/NCI Cancer Center Support Grant P30-CA016672 (to the Bioinformatics Shared Resource), NIH/NCI T32 Award CA009666 (to C.M.G.), The University of Texas Southwestern Medical Center and MD Anderson Cancer Center Special Program of Research Excellence (5 P50 CA070907), NIH/NCI award R01-CA207295 (to L.A.B.), NIH/NCI award U01-CA213273 (to J.V.H. and L.A.B.), NIH/NCI award U01 CA231844 (to T.G.O.), award P30CA042014 (to the Huntsman Cancer Institute), the Department of Defense award LC170171 (to L.A.B.), the ASCO Young Investigator Award (to C.M.G.), generous philanthropic contributions to The University of Texas MD Anderson Cancer Center Moon Shots Program (to J.V.H., J.W. and L.A.B.), The University of Texas MD Anderson Cancer Center Small Cell Lung Cancer Working Group, Abell Hangar Foundation Distinguished Professor Endowment (to L.A.B. and B.G.), The University of Texas MD Anderson Cancer Center Physician Scientist Award (to L.A.B.), The Hope Foundation SWOG/ITSC Pilot Program (to P.R. and L.A.B.), an Andrew Sabin Family Fellowship (to L.A.B.) and Rexanna’s Foundation for Fighting Lung Cancer (to J.V.H. and L.A.B.).
Author information
Authors and Affiliations
Contributions
C.A.S., C.M.G. Y.X. and L.A.B. conceived of the project, analyzed and interpreted the data and wrote the manuscript. S.S., V.S., V.B., P.R., J.Z., B.G., J.d.G., S.G.S., J.A.R., M.D.C., T.G.O. and J.V.H. contributed to acquiring the data. J.F., C.M., N.K., J.S. and I.W. performed the pathology review and analysis. M.B. and J.W. contributed to analysis and interpretation of the data. P.M.H. collected liquid biopsies from the patients. H.T. coordinated the patient protocols. P.R., J.Z., B.G., J.d.G., S.G.S., J.A.R., M.D.C., T.G.O. and J.V.H. provided administrative and/or material support. All authors contributed to the writing, reviewing and/or revising of the manuscript.
Corresponding author
Ethics declarations
Competing interests
L.A.B. serves on advisory committees for AstraZeneca, AbbVie, Genmab, BerGenBio, Pharma Mar SA, Sierra Oncology, Merck, Bristol-Myers Squibb, Genentech and Pfizer and has research support from AbbVie, AstraZeneca, Genmab, Sierra Oncology and Tolero Pharmaceuticals. J.V.H. serves on advisory committees for AstraZeneca, Boehringer Ingelheim, Exelixis, Genentech, GlaxoSmithKline, Guardant Health, Hengrui, Lilly, Novartis, Spectrum, EMD Serono and Synta, and has research support from AstraZeneca, Bayer, GlaxoSmithKline and Spectrum and royalties and licensing fees from Spectrum. Otherwise, there are no pertinent financial or non-financial conflicts of interest to report.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CDXs exhibit common SCLC markers and mutations that are maintained over multiple generations.
a, Histological analysis of CDX tumors are consistent with SCLC. Scale bar = 100 µM. b, Patient expression of NCAM and TTF1 by staff pathologist review of diagnostic sample matches CDXs. c, Presence of parenchymal brain metastasis, confirmed by staff neuroradiologist and treating physician review, in the cerebellum (indicated by dashed circle) of the patient from which MDA-SC39 was derived. d, Genomic alterations in CDXs. Top panel: mutation load; middle panel: somatic mutations and genomic gain/loss status; lower panel: type of base-pair substitution. e, Mutational status of common SCLC genes and others unique to each CDX are maintained over multiple CDX passages in three separate models. f, Expression heatmap for ASCL1- and NEUROD1-associated genes. b, CDX and PDX models derived from patient SC49 exhibit similar patterns of expression for common SCLC markers, including loss of TTF1 expression. These experiments were repeated in three independent tumors from each model. Scale bar = 100 µM.
Extended Data Fig. 2 ITH among SCLC molecular subtypes.
a, t-SNE visualization of NE gene expression status in all CDXs. b, t-SNE visualization of cell populations from biological replicates of MDA-SC39s and MDA-SC16r obtained from tumors grown in the same passage, but different mice. Note mixing of cell populations indicate that clustering is not due to variations in replicate. c, Heatmap analysis of NE gene expression indicating that all CDXs are considered high neuroendocrine subtypes. d, Expression of ASCL1 and NEUROD1 in all CDXs by both violin plot to indicate range in expression and feature plot to show abundance. e, Violin plots indicating expression of MYC family members in the CDXs. Each dot represents one cell and the violin curve represent the density of the cells at different expression levels. f, EMT score is elevated within MDA-SC39s and MDA-SC49r, which corresponds with increased expression of VIM and decreased EPCAM. In a, b, d, e, and f, n=2,000 cells each.
Extended Data Fig. 3 Validation of cluster calls and visualization.
a, Silhouette analysis to determine cluster number in each of the eight CDXs. b, UMAP visualization of the clusters in all CDXs. c, Barplot of variations of absolute normalized enrichment scores (NES) for hallmark pathways in GSEA analysis in sensitive clusters (blue) and resistant clusters (red). The variation of pathway enrichment is higher in resistant clusters than sensitive clusters by one-sided Wilcoxon rank sum test (P=2.9e-6; n=21 pathways).
Extended Data Fig. 4 CDX copy number and expression of DNA repair genes between clusters.
a,b, Inferred copy number between clusters in MDA-SC16r (a) and MDA-SC49r (b). c, Expression heatmap of genes associated with DNA repair in all CDX clusters. d, Violin plots indicating range of expression of several therapeutic targets within individual clusters. AURKA, AURKB and DLL3 were relatively unchanged between clusters. MDA-SC4s: n=978, 1,022 cells for clusters 1-2; MDA-SC39s: n=1172, 828 cells for clusters 1-2; MDA-SC68s: n=733, 704, 563 cells for clusters 1-3; HCI-008s: n=596, 1,404 cells for clusters 1-2; MDA-SC49r: n=683, 317, 652, 348 cells for clusters 1-4. Each dot represents one cell and the violin curve represent the density of the cells at different expression levels.
Extended Data Fig. 5 Validation of CTC identification within a patient liquid biopsy by positive expression of epithelial, NE and SCLC genes.
Percentage of cells expressing epithelial, NE genes (for example, UCHL1, NCAM1, SYP, and CHGA) or SCLC lineage-specific genes (for example, ASCL1, NEUROD1, etc.) in the CTC population and non-CTC populations.
Extended Data Fig. 6 Emergence of a mesenchymal cell cluster following cisplatin-treatment.
Violin plot of VIM (a) and EXPCAM (b) expression in the clusters of MDA-SC68s vehicle and cisplatin-treated CDXs. MDA-SC68 vehicle: n=733, 704, 563 cells for clusters 1-3; MDA-SC68 cisplatin: n=635, 489, 71, 467, 338 cells for clusters 1-5. Each dot represents one cell and the violin curve represent the density of the cells at different expression levels Source data.
Supplementary information
Source data
Source Data Fig. 1
Statistical Source Data
Source Data Fig. 2
Statistical Source Data
Source Data Fig. 3
Statistical Source Data
Source Data Fig. 4
Statistical Source Data
Source Data Fig. 5
Statistical Source Data
Source Data Fig. 6
Statistical Source Data
Source Data Extended Data Fig. 1
Statistical Source Data
Source Data Extended Data Fig. 2
Statistical Source Data
Source Data Extended Data Fig. 3
Statistical Source Data
Source Data Extended Data Fig. 4
Statistical Source Data
Source Data Extended Data Fig. 5
Statistical Source Data
Source Data Extended Data Fig. 6
Statistical Source Data
Rights and permissions
About this article
Cite this article
Stewart, C.A., Gay, C.M., Xi, Y. et al. Single-cell analyses reveal increased intratumoral heterogeneity after the onset of therapy resistance in small-cell lung cancer. Nat Cancer 1, 423–436 (2020). https://doi.org/10.1038/s43018-019-0020-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-019-0020-z
This article is cited by
-
Cellular hierarchy insights reveal leukemic stem-like cells and early death risk in acute promyelocytic leukemia
Nature Communications (2024)
-
A telomere-targeting drug depletes cancer initiating cells and promotes anti-tumor immunity in small cell lung cancer
Nature Communications (2024)
-
Robust detection of clinically relevant features in single-cell RNA profiles of patient-matched fresh and formalin-fixed paraffin-embedded (FFPE) lung cancer tissue
Cellular Oncology (2024)
-
Evolutionary trajectories of small cell lung cancer under therapy
Nature (2024)
-
Orchestrating smart therapeutics to achieve optimal treatment in small cell lung cancer: recent progress and future directions
Journal of Translational Medicine (2023)